A most chronic depression
My mental health file whirs to life in 1969 in Cambridge, Massachusetts. I'd recently left Opus Dei, the Catholic religious order to which I'd committed my young soul, and a major depression had followed. The records printed below are out of the mouths of my many caretakers; they chronicle my treatment at various medical offices and psychiatric clinics in the Boston area, from then until 2012.
How did I come by them? As I headed into a depression two years ago, a friend who was helping out thought it would be useful to see my records, so I asked for them. Why publish them now? Certainly not because I think these extracts from my treatment notes display any special literary facility or reveal an exceptionally interesting psyche, nor because I intend the slightest scandal to be visited on my therapists, employers, or insurance company. All proper names have been altered.
Our distractible human intelligence needs as many ways of talking about depression as can be provided--that's all. Plus, given the longevity of this particular demon, it seems important to try to squeeze some insight from the mass of words and array of prescription drugs applied against its havoc. Even the most comprehensively bureaucratized medical knowledge can be made to speak, if only we are willing to listen closely to the blank spaces, the paraphrases. Even acronyms have feelings.
A note on medications: Fifty-plus years into the Antidepressant Age, it's still not clear that drugs are better than placebos. There aren't many long-term studies of efficacy or side effects, and the FDA requires surprisingly few trials before approval. Each of the drugs comes with a more or less plausible scientific explanation for why it should work. But all we know is that some people get better after taking them, some people don't, and some people get better without taking them.
Of course, from a patient's point of view, this is all moot. If you're jumping out of your skin and the doctor says to take some pills, you take them. In my case, none of them worked spectacularly well. But only a couple had intolerable side effects or made the depression worse.
The following records have been lightly edited. Spelling errors
have been corrected, abbreviations standardized, and doctors' names changed.
-The Editors
August 16, 1969
Trigg Clifton, MD/MB
Harvard University Health Services, Psychiatric Clinic
Cambridge, Massachusetts
Patient is seen as a courtesy visit because he is no longer actually eligible for consultation here, as he graduated here from the college [Harvard] in June of this year. He has plans to attend Columbia Graduate School.
He comes with very intense questions regarding Catholicism. In the last several months he has begun to question increasingly whether he can support a body of thought which stresses orthodoxy and lack of investigation. He approaches the problem with me and with himself quite intellectually, but he is indeed, in spite of intellect, feeling in much emotional turmoil over this. Support was given to him to move towards a middle ground, which, in his style, is very hard for him.
He has felt frightened of the loss of the church, and, therefore, it was clarified that he need not give up the church, or an organization to which he belongs in the church, to pursue his questioning, and that he would not be able to be content in any position he took until he opened up the questions with himself and others. He was also concerned that some of his actions have been inappropriate, and I did not feel that they were inappropriate save that they were indicative of a young man in considerable turmoil over some very important questions in life, and this was stated to the patient.
He will be talking with several priests and may indeed, when he gets to Columbia, seek psychiatric help for the personality problem of a semi-crippling obsessive-compulsive personality, i.e., he is often paralyzed by self-doubts and inability to be decisive.
At the end of the interview he questioned whether his difficulties would make him draft deferrable, and I stated that I did not think so.
DIAGNOSES: Adjustment Reaction of Adolescence in an obsessive-compulsive personality.
September 30, 1970
Trigg Clifton, MD/MB
Harvard University Health Services, Psychiatric Clinic
Cambridge, Massachusetts
The patient has been in New York City in the graduate school at Columbia, but really had a severe obsessive breakdown in functioning, necessitating his dropping out of school. He was in treatment about eight months in New York City at the clinic, but left treatment for reasons that are not clear approximately two months ago. He is now up here, hoping to pull himself together, and plans to take six courses through the Extension [School].
He came to see me to reestablish contact, and to question if he could get into treatment. I am aware that his treatment has been difficult for him, but see him as a very troubled man, and I would venture to say probably sicker than an adjustment reaction of adolescence--more likely borderline personality with obsessive-compulsive features. Obviously he could not be treated at this clinic, and he is uncertain whether he wants to get into treatment at all. I told him that if he did, he should feel free to get in touch with me and I would find him a clinic in the area.
He is not suicidal, and there are no signs of acute decompensation.
August 17, 1981
Jennifer R. Hornstein, MD/MB
Harvard University Health Services, Psychiatric Clinic
Cambridge, Massachusetts
This was the first Mental Health Service visit for this 33-year-old young man who is currently working as a receptionist for the Center for International Studies. He presents with the chief complaint, "I am worried about my medical condition. I tried to go to the clinic but wasn't sure whether I should go. I think these symptoms are getting worse."
The patient is a neatly groomed, articulate, extremely anxious young man who presents with a history of anxiety for the past four months. He states that since April, when he became 33, he has been increasingly anxious with difficulty falling asleep, midnight awakening and early morning awakening. He says that over the past few weeks he has only been able to sleep approximately five hours per night. He describes compulsive eating and heavy intake of "junk foods." He says that he has gained about eight pounds since April. He reports a loss of energy, anhedonia, and a decrease in sexual interest as well as a difficulty in obtaining erections. He denies suicidal or homicidal ideation. He denies history of hallucinations or delusions. He denies confused episodes. Furthermore he denies drug or alcohol intake.
Over the past four months, he has become increasingly fatigued and unable to cope with his current situation. He says that he is reminded of a period when he was 21, when he decided to leave the Catholic religious order which he had committed himself to.
Since leaving the Order, an Order for laymen who dedicated themselves to chastity and poverty, he has not been able to commit himself to any pursuits. Over the past several months, he has gone from one therapist to another and has recently been involved with primal therapy. His involvement with primal therapy has lasted six months, but he now says that he would like to pursue other avenues, and is unable to explain why. He also saw several therapists, including a therapist at the Harvard Community Health Plan who prescribed some Valium for him, which he takes at a dose of 2.5 to 5 mg by mouth as needed to a maximum of 5 mg at night. He says that this occasionally helps him sleep but it has not relieved his anxiety in the long term.
He also states that approximately a month ago, he saw a therapist who prescribed Sinequan for him. He took several doses of this but says that it did not help and he discontinued this medication and has not seen the therapist since.
Patient reports symptoms of severe anxiety and obsessionality. He reports being unable to make a decision about anything, even whether he will be able to continue therapy or not. He is worried that there might be something medically wrong with him, and has made an appointment to see Dr. Shepard for Wednesday. He is not sure what he would like from me at this time, other than some instant relief, or reassurance that his symptoms will not get much worse. He is worried he will become so tired that he will not be able to return to the clinic or even walk across the campus to see me for our next appointment.
I suggested that he come in again for further evaluation. I will see him Friday and then refer him for the two weeks that I am on vacation. He says that he does have friends who will visit him so that he is not entirely isolated. We also discussed the possibility that he may come in to Walk-In at any time during this week, or that he may call the Emergency Room if he feels the need.
My initial impression is that this young man presents with an agitated depression or anxiety attacks. He denies hyperventilation or palpitations. However, he does describe some phobic symptoms in that he is worried that he will stay in his house and not be able to leave. I did not think that acute hospitalization was necessary at this time. I discussed the possibility of beginning antidepressants, which may be helpful in treatment of both the depression and the panic attack symptoms. However, I also advised him that we would need further work up before beginning medication.
This patient appears to have difficulty in following through with appointments in the past, and I discussed the necessity of continued evaluations and appointments in order that the evaluation be completed. My plan is to see him Friday and refer him for continued evaluation during the next two weeks.
August 26, 1981
Jeffrey F. Parsnip, MD/MB
Harvard University Health Services, Psychiatric Clinic
Cambridge, Massachusetts
As arranged by Dr. Jennifer R. Hornstein, I met with Mr. Scialabba today. My assessment, which is in agreement with Dr. Hornstein's, is that this man suffers from a rather severe endogenous depression superimposed on a schizoid personality.
Symptoms of major depression that he admits to, which have been present for two to four months, include frequent early morning awakening; constipation; absent interest in sex; diurnal variations, with the early morning the worst; increased appetite with eight pounds weight gain; and profoundly decreased energy. I do not think that he suffers from true panic attacks, but rather somatic symptoms of anxiety.
The only family history of emotional illness is a first cousin, mother's brother's son, who committed suicide at age 21. There is no family history of alcohol abuse.
Certainly the chronic decline in functioning from his levels of a decade ago is disturbing. After graduating Harvard in 1969 with a group 2 average, he flunked out of Columbia, where he was studying history. Since then, he has spent a number of years working as a social worker in a local welfare department, but he says that this job was largely paper work. He has been working as a receptionist at Harvard for the last year. He has no close friends and although he has had sexual intercourse he has not had close or enduring relationships.
He describes his mother as having been dominating, although very nervous, and his father as a timid, weak man. Father held an office job and mother was a stitcher. There is one brother who is taking night school courses at Suffolk Community College and works in the Public Works Department. Thus, the patient greatly exceeded the level of the success of his family, simply by going to Harvard and doing well there.
I wonder whether part of his subsequent decline is attributable to oedipal fears which his success represented. He now has multiple fears of losing control, which he fantasizes would result in his becoming passive, being unable to hold a job, going on welfare or into a hospital and not being able to take care of himself. This may be a regression prompted by his earlier successes.
He describes having wanted to be a priest from second or third grade, and such a role was highly respected within his community. He currently has fears that his turning away from religion may have been a mistake and that he could be damned to hell for this. He also fears punishment for compulsive masturbation, which he says he engaged in daily for ten years prior to his loss of sexual urges these last few months.
Given the chronic schizoid adaptation, the apparent decline in function over a ten-year period, and his albeit culturally sanctioned interest in religion and philosophy, I looked hard for a thought disorder but was unable to satisfy myself of the presence of one. His functioning within the last four months is clearly discontinuous with his chronic level of functioning over the last ten years. During these four months he has classic signs of an endogenous depression of severe degree, with agitation.
Physical examination has been performed and is normal. CBS, SGOT, urinalysis, and thyroid function tests are normal. BUN is marginally elevated. Dexamethasone suppression test is negative.
It is my assessment that he will likely benefit with a course of tricyclic antidepressant therapy. I began discussing this with him today and will meet with him for further discussion tomorrow, and probably start him on desipramine at that time.
July 6, 1987
Melinda R. Maron
McLean Hospital, Ambulatory Care Services
Belmont, Massachusetts
INTAKE REPORT
Chief Complaint: Patient saw Dr. Mason once, and he referred him here because of financial concerns. Generally feels emotionally fragile. Is high-strung and unable to make life decisions. Feels he's drifting professionally. "Ridiculously over-qualified for what he does!"
History of Present Problem: Early traumatic break from religious tradition, Catholicism, at age 21 and feels that he's never really recovered.
Family Information/Current Living Situation: Lives alone. Parents and one brother live in the area.
Medical History/Current Medications: Physically in good health--not "bursting with energy." No meds. No alcohol or drugs.
Previous Outpatient Treatment: Yes--few times in the '70s.
Previous Hospitalizations: None.
Additional Psychiatric History: No. One cousin had psych problems and suicide at age 22.
Insurance Coverage: HVHP
Impression at Intake: Patient found it very difficult to talk, seemed very constricted and upset.
December 30, 1987
Melinda R. Maron
McLean Hospital, Ambulatory Care Services
Belmont, Massachusetts
TREATMENT PLAN
Problem No. 1: Depression as shown by social isolation, inability to make career decisions, and overwhelming feelings of guilt.
Goal (long term): Reduce feelings of guilt, paralysis about decision, and social isolation.
Objectives (short term): Patient will understand more about the connection between his behavior and his depression. Patient will feel less despair and guilt about his choices.
Expected Achievement Dates: Long term--6/90. Short term--9/88.
Specific Plans: Individual psychotherapy, once per week.Psychopharmacology with behavior therapy, once per month.
Problem No. 2: Personality disorder with obsessive-compulsive style and depression that contribute to his paralysis and lack of intimate relationships.
Goal (long term): Modification of obsessive-compulsive defenses.
Objectives (short term): Patient will become more flexible and tolerant of himself and his affects.
Expected Achievement Dates: Long term--6/90. Short term--9/88.
Termination Criteria: Reduce depression. Modification of rigidity of obsessive-compulsive personality disorder.
DIAGNOSIS SUMMARY
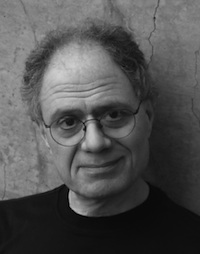
Identifying Data: Mr. Scialabba is a 39-year-old white single male who works full time in a clerical position at Harvard University. He graduated from Harvard in 1969. Mr. Scialabba described himself as growing up a devout Catholic, but he left the church after graduating from Harvard. He was referred by Dr. David Mason, attending psychiatrist at McLean.
Data Source: Mr. Scialabba has been seen by Roberta Tate, LICSW, in once-a-week psychotherapy since 8/87. The patient was assessed on 7/23/87, by Dr. Juan Durendal, and some of the data in this report has been taken from that assessment.
Chief Complaint: Mr. Scialabba described himself as "emotionally fragile, high-strung, and unable to make life decisions. I am ridiculously over-qualified for what I do; I feel stalled in my life and want to know if there is a medication that could help me."
History of Presenting Problem: Mr. Scialabba dates his psychiatric symptoms back to age 17 when he developed incapacitating anxiety when he had any sexual impulse and he would have guilty ruminations that disrupted his usual activities. He went to a priest who told him he would be responsible to God for the patient's sexual impulses, and the anxiety episodes stopped. Mr. Scialabba also joined a very devout all-male Catholic organization called Opus Dei, and he became very involved in that organization during his undergraduate years at Harvard. He felt a missionary zeal about converting others and involving them in Opus Dei. Mr. Scialabba describes his commitment as "intense, demanding, and lifelong." After four years of college he "lost all belief in Catholicism."
Mr. Scialabba describes his leaving the church and Opus Dei as extremely difficult, and he described an episode of confusion and perhaps of depersonalization in which he didn't know what he was going to do, but he went into a meeting of Opus Dei and tried to speak about his loss of faith. Instead he became agitated and had to be led from the room. Mr. Scialabba feels he has never recovered from this emotional upset. He describes the time leading up to his departure from Opus Dei as the most intensely meaningful, exciting time in his life, when he felt that all of life and intellectual and philosophical pursuits were open to him.
He attempted graduate school at Columbia in European intellectual history as well as Harvard Law School, but he dropped out of both because whenever he attempted to do serious work in philosophy or intellectual history, he would become unbearably agitated and have to stop. He returned to Cambridge after one year at Columbia and has remained here ever since.
Mr. Scialabba has had a series of "undemanding and unrewarding jobs" such as substitute teaching, welfare social worker, and currently is a receptionist/staff assistant at Harvard's Center for International Studies. Mr. Scialabba, during the last 5 years, has done a fair amount of freelance book reviewing for the Village Voice and a journal called Grand Street.
May 28, 1996
Bert Milliner, PhD, MPH
Harvard University Health Services, Psychiatric Clinic
Cambridge, Massachusetts
Mr. Scialabba is 48, born in Boston and grew up in East Boston. His parents are living, married, and live in East Boston. He is the second of two with an older brother. He is single, never married, in a relationship with Janice at 45 or 46, and she is an editor at an academic press and writing her dissertation. The relationship has been ongoing for 2.5 years, and Mr. Scialabba has no children. He does not have a lot of friends but has a few. He has a master's degree in history, is a building manager at the International Studies Center, but spends much time in freelance book reviews. He has been at the International Studies Center for 16 years. He lives in Cambridge alone, does not smoke, does not drink, does not use any drugs, has no history of these, no family history, and in terms of psychiatric history, he had a first cousin who committed suicide at 20. He notes his mother is a severely dysthymic and severely obsessional person, diagnoses which have been applied to him by an eminent psychiatrist and which seem right to him. He has no physical problems and takes Zoloft, up to 250 mg at this time, although he was on a maintenance dose for three years of 50 mg. He does not get very regular exercise, jogs once a week, and does 5-10 minutes of calisthenics each morning. In terms of psychological treatment, he has been in psychotherapy a number of times, he would say unsuccessfully, only once for more than a year. He has had two clinical depressions in the last 15 years, both for several months, but pretty awful. He has seen Dr. Woodcourt for about five years.
He presents today noting that he was a little shaken by the episode six weeks ago. He does not know what brought it on, noting he wound up in psychodynamic therapy three years ago after five years. It was someone he liked but it didn't seem to help. He thinks his concerns are partly biochemical and he is grateful for Zoloft.
He has come across a number of articles that say cognitive therapy has the highest success rate, he has read Feeling Good and one or two books by Aaron Beck, although he was rather scornful of these and still is. He is sympathetic to psychoanalytic ideas, but he has been humbled by these depressions.
The overall problem he notes was that he was a very devout Catholic, part of a religious order, which he left at 21 during the summer between college and graduate school. He was so agitated he had to drop out of graduate school. Seemingly, the pieces of his life never came back together. He did not feel able to do any intellectual work, never resumed his life again. When he tried to read philosophy or political history, he was unable to focus, felt a certain background tension. For the past 15 years, he has been in literary criticism, written about 150 book reviews, won a ational award. However, it is not the same as having a career, and he still feels kind of disabled. On a micro-level, he has always been very obsessive, fretful, replaying decisions, defensive, and feeling he has to defend himself against imagined threats, although he has never been delusional or psychotic.
I explained our more focused and briefer time frame and noted if he was going to begin something that would be longer term, he'd want to actually change his basic affect. He never went back to graduate school because he didn't think he could handle it, and although he would not choose to do so now, he would want to feel he could. He seemingly had felt that if he pulled out all the stops, he would freeze up. If we had only a few sessions, he would want me to convince him to decide on whether to go on in terms of therapy and what kinds of therapy it would be or what realistic goals he might set.
I briefly explained my view of cognitive therapy as involving the belief system of both the therapist and the patient and involving the belief that one's cognitions could affect one's experience and one's feelings. He said this sounded reasonable to him and that he was ready to try anything. We set a follow up for June 17, at 10 a.m.

May 16, 2005
Allan Woodcourt, MD
Harvard University Mental Health Services
Cambridge, Massachusetts
In the past three days he's sunk into a severe agitated depression again. He feels worse than he's ever felt. He feels like pacing all day, and has trouble sleeping, though he feels exhausted. It's getting harder and harder to eat. He thinks of death, but would not kill himself, and hasn't been making plans. He wants to go to a "rest house." We agreed that hospitalization would not help because of the environment. He has nobody he can turn to. His girlfriend is too busy to take time off. He hasn't called her and told her what he's going through, but I encouraged him to. He doesn't have faith in the Effexor, but it worked for years, and he's relapsed at least partly because he lowered the dose. We agreed he'd increase to 150 mg immediately. He'll also use lorazepam during the day, which has helped before, and olanzapine at night, for its antidepressant-augmenting possibility. He'll be back to me tomorrow, late in the day, and knows about the availability of urgent care.
June 9, 2005
Allan Woodcourt, MD
Harvard University Mental Health Services
Cambridge, Massachusetts
He says that, within the last 24 hours, the agony is a bit less, but he doesn't trust the feeling. He still has a worm's eye view of himself and his life. It turns out that he won't have to be housed in a corner of his boss's office in the new building, but will have a very small office of his own, which is a huge relief. He'll have to come to work on time (11 a.m.) in the new location. He's not used to that. In his old job, he was able to get the little which needed to be done accomplished on a very flexible schedule. He chides himself for his "immaturity" in that he has a menial job, etc. But at this point, he's still not in touch with what new freedom he might like which more "maturity" would give him. He'll continue to see Dr. Pingloss in June and, when I'm back in July, we'll work on another referral for him. He'll see Ms. Lewis next week (June 15) for monitoring.
He found his consultation with Dr. Morrell helpful, partly because the appointment was longer, and "I was able to tell my whole story."
September 21, 2005
Luke Honeythunder, MD
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Electroconvulsive Therapy, Treatment #1
I. Subjective/Objective
Clinical Assessment: I met with him & brother as outpatient. I again discussed with him the ECT benefits & risks, with the latter including death, cognitive problems, cardio-pulmonary problems, & others. He understood and agreed.
Suicidal Assessment: He denies suicidal or destructive ideas, intent, plan.
Memory Assessment: Cognition intact.
II. ECT
Observations: He tolerated the procedure well.
III. Post ECT
Observations: By 65 minutes after ECT, he was recovering well, cognitively and physically.
September 23, 2005
Luke Honeythunder, MD
Beth Israel Deaconess Medical Center
Boston, Massachusetts
Electroconvulsive Therapy, Treatment #2
I. Subjective/Objective
Clinical Assessment: "Depressed" mood with dysphoric affect. Asked about when to expect improvement in mood. Psychomotor retardation.
Suicidal Assessment: No SI voiced.
Memory Assessment: Grossly intact for recent events.
II. ECT
Observations: Patient tolerated ECT well.
III. Post ECT
Observations: Within 30 minutes after ECT, patient was recovering well physically (with nausea) but continued to have difficulty with orientation. He notes he is still depressed.
October 18, 2005
Allan Woodcourt, MD
Harvard University Mental Health Services
Cambridge, Massachusetts
He's now had about eight ECT treatments. He's having significant short-term memory problems, and forgot his appointment with Ms. Trone, and forgot that he had any appointments scheduled with me. His brother called me and we straightened that out. He says the agony is gone, but that he feels "numb" and unmotivated. He's not working now, and spends much of his time in bed. He is beginning to read a bit, and we talked about something in the New York Review of Books. He says he has little appetite. He's seeing friends, "a bit," but finds it hard with his memory problems. He's not been seeing Dr. Gusstav during the series of ECT, and thinks he may not be a good match for him anyway.
November 3, 2005
Allan Woodcourt, MD
Harvard University Mental Health Services
Cambridge, Massachusetts
He says, for the first time in at least six months, "I'm alright." His mood is definitely better. He's dressed better, and even smiles a bit. He still has decreased concentration and motivation, but he's eating better, and is doing some socializing. He went to a friend's birthday party last weekend, and is going to a concert this weekend. He'll be continuing the ECT treatments, twice weekly, for now.
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
February 16, 2007, 7:33 p.m.
From: George Scialabba
To: Allan Woodcourt, MD
Subject: zoloft
I've started to see someone and I'm a little concerned about the effect of Zoloft on my libido. Do you think it would be all right to go down gradually to 100 mg? --George
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
February 18, 2007, 11:05 a.m.
From: Allan Woodcourt, MD
To: George Scialabba
I'm extremely reluctant to see you taper the Zoloft, but I can well understand your frustration with the current situation. When I get back to work on Tuesday, maybe we can set up an appointment to brainstorm about what to do. --Al Woodcourt
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
February 20, 2007, 1:38 p.m.
From: George Scialabba
To: Allan Woodcourt, MD
OK, maybe you're right. I suppose I shouldn't take any unnecessary risks. Do you feel the same way about 150 mg? --George
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
February 20, 2007 5:02 p.m.
From: Allan Woodcourt, MD
To: George Scialabba
I doubt that going down to 150 mg would improve your sexual function very much if at all, and it would increase the risk of a relapse, so I wouldn't be in favor of that either. --Al Woodcourt
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
February 20, 2007, 5:19 p.m.
From: George Scialabba
To: Allan Woodcourt, MD
Ok, better safe than sorry. I'll stay at 200 mg. --George
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
August 1, 2008, 9:30 a.m.
From: Allan Woodcourt, MD
To: Deborah Simmons, MD
Subject: George S.
We share George Scialabba, who has a history of devastating depressions. He's been well for the past two years, but before that he was nearly dead, and was only rescued by ECT, which he had at the Beth Israel Deaconess Medical Center. He has a therapist whom he sees every other week, and I see him only every 4-6 months. He does well on his sertraline 200 mg [Zoloft], but he's always tempted to cut it back. My role is to point out to him what a big mistake that would be.
He's relied on me for many years at University Health Services, but his relationship to me is ambivalent. He felt very attached to Dr. Cindy Shepard and feels very comfortable with you. I am wondering if you would take over monitoring his sertraline after I retire? If his depression returns, you'd have to refer him out, and my own thought would be that he should go back to ECT early rather than after many drug trials. I'd be happy to be available to consult about him by email or by phone.
If you don't feel comfortable with this plan, please don't hesitate to say so, and I'll hook him up with someone down here before I go.
Thanks for considering. --Al
= = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = = =
August 1, 2008, 9:33 a.m.
From: Deborah Simmons, MD
To: Allan Woodcourt, MD
I think I have an open and thoughtful relationship with him and would be happy to monitor his meds. He is having a sleep study soon since he has a sleep disorder that is not entirely clear to me. --Deborah
July 6, 2012, 11:15 p.m.
Lenora Giles, LICSW
Harvard University Health Services After Hours Urgent Care Clinic
Cambridge, Massachusetts
Reason for Call: Patient called the After Hours Urgent Care Clinic at 11:15 p.m. Friday evening requesting help for an "emergency." He reports being "seriously depressed and suffering, in a tremendous amount of pain." When asked if he felt safe, he replied, "this is an emergency, I don't think I would do that but it can't get much worse."
Patient of mental health for over twenty years with history and treatment of major depression, including ECT. Had recently "foolishly" (his report) began tapering his medication. In the last few days he has felt significantly worse, not sleeping, not eating, in acute "pain and suffering." Denies any ETOH use. His initial request was for medication. Based on what he was reporting, my recommendation was that he go to Cambridge Hospital, saving the step of a visit to University Health Services. I suggested to him that would be the most efficient way for him to be evaluated for medication and potentially inpatient. He agreed and was relieved. He asked me to speak with his girlfriend who was with him. She had come over to "support him" and found him "curled up on the bed, crying."
They will go together to Cambridge ER, she will stay with him and present her observations to the evaluating clinician. They will ask the hospital to call and report the disposition to AHUC.
July 23, 2012
Joanne Levy, MD
Harvard University Mental Health Services
Cambridge, Massachusetts
Chief Complaint: "I have been feeling very depressed."
History of the Present Illness: Mr. Scialabba is a 64-year-old self-described writer and academic coordinator at Harvard who has a 30-year history of major depression. He has had at least 5-6 major depressive episodes in his life, the most recent of which started in the spring of this year following a taper of his Zoloft medication from 200 mg to 100 mg daily. He described feeling very irritable a few weeks after starting the taper (which was started by his PCP after patient voiced concern over decreased libido), but that the onset has been somewhat gradual and insidious in general. Mr. Scialabba began seeing Dr. Filep in Behavioral Health in January of 2012 and tapered his Zoloft slowly. By June of 2012 he began feeling increasingly depressed. The Zoloft was restarted, but the decline continued. Was hospitalized about 2 weeks ago in Everett (went to Cambridge Health Alliance ER) for 3 days, where Ativan was started with some effect on sleep and Zoloft was increased further to 100 mg daily. Continues to have anxiety.
Last saw Dr. Filep on July 10, 2012, and, at that time, the Zoloft was increased from 100 mg to 200 mg daily. Patient came in today with a close male friend, John, who feels strongly that the patient cannot wait for his symptoms to improve and was concerned that the patient would be headed towards a severe depression if there was not an urgent intervention. Currently, patient endorses low energy, depressed mood, difficult focusing, poor sleep, agitation, as well as a tightness in his chest and a "flaming sensation within me" (which is reportedly characteristic of his past episodes). Does not have suicidal thoughts currently, but has wished in the recent past that he would be able to go to sleep and not wake up. Has many friends and supports here in Boston, who reportedly give him hope for the future. Discussed options for immediate intervention, as well as longer-term medication/treatment options. Patient does not feel that he needs to be hospitalized at this time. Suggested increasing the Ativan for agitation and continuing to give some time for the increased dosage of Zoloft to take effect. Also discussed ECT, as that has worked in the past, though this clinician feels it is premature to discuss this as patient was maintained on Zoloft for more than 5 years with no reoccurance of his depression in the past and he is still in the middle of an upwards titration.
Past Psychiatric History: At least 5 major depressive episodes in the past with very chronic symptoms (per past notes, symptoms resistant to a multitude of treatment at times), one prior inpatient hospitalization just this month (July 2012), no prior suicide attempts, history of ECT in 2005 which was very effective. Past medications have included: Parnate, desipramine, nortriptyline, Effexor XR, Wellbutrin, Adderall, Strattera. Saw Dr. Woodcourt at Harvard University Health Services for many years (at least since 1993-2008). States that he has an outside therapist who is an analyst that he sees every 2 weeks for the past 5 years, but that the therapist is on vacation for a month and that he has not seen the treater in quite some time. No history of a prior manic episode or psychotic symptoms.
Past Medical History: (Per chart) sleep apnea, benign prostatic hyperplasia, impotence, and sexual dysfunction.
Social History: Works as a coordinator at Center for Government and International Studies at Harvard. Has been able to work recently, but in the past has missed many months of work due to depression. Lives alone in Cambridge. Is very close to his brother and notes that he has two other close friends who check in on him regularly (one of whom is present today with him). Denies having access to any weapons in the home or otherwise. Likes to write and has several published pieces.
Family History: Both of patient's parents were reportedly dysthymic, maternal grandmother had ECT, first cousin suicided at age 21.
Detailed Mental Status Exam: Decently groomed, thin, frail man. Discusses his symptoms and suffering openly.
Treatment Review: Discussed a goal of decreasing patient's mood symptoms and anxiety from a 8/10 to at least a 5/10 over the next week.
Current Plan:
1. Add a second dose of Ativan in a.m. when anxiety is at its worst (0.5 mg)
2. Follow up again this week (July 27, 2012) to assess if the symptoms have improved due to medication compliance with Zoloft and addition of Ativan dosage. Was instructed to call (during business hours) or go to the nearest emergency room for help if he feels actively suicidal or unsafe at home.
3. Will consider ECT consult if symptoms worsen or if no better in 1-2 weeks.
4. Patient will resume care with assigned clinician Dr. Filep when she returns from vacation.
[AFTERWORD]
I am as puzzled and frustrated by the above records, and by the rest of my psychiatric file, as any casual reader could be. So much earnest effort, so much expert knowledge, so little success. The world's most common disease is still this opaque.
Having read half a dozen compelling depression memoirs--Styron, Jamison, Millett, Solomon, Kaysen, McMurtry--I was skeptical, when The Baffler proposed publishing extracts from my file, that there was much more to say. Maybe there isn't, at least not in that register. But maybe it's enough just to keep talking.
Let me bring this melancholy chronicle up to date. The last record printed here is dated July 2012. Things remained bad through August and September. In early October I began a three-month medical leave of absence, with pay; I had taken a similar leave in 2005, when the depression was at its worst. Harvard has a generous provision for medical leave, perhaps because of the presence of a strong union, the Harvard Union of Clerical and Technical Workers (HUCTW). Once again, the medical leave made possible a course of electroconvulsive therapy, this one only about half as long as before.
What would have happened if I had not received those medical leaves is something I'd rather not think about. At the least, a psychological ordeal would have eventuated in a financial calamity. The combination of an enlightened employer and a strong union is one that ever fewer Americans enjoy. Universal financial security is probably the single best countermeasure to the depression epidemic. It would certainly be more effective and more humane--and even, perhaps, cheaper--than providing antidepressants and ECT.
Since early 2013, I've been depression-free. A good therapist has helped, as well as a few sweet professional successes. A doctor once cautioned me that after three major depressions the probability of a recurrence approaches 100 percent. She didn't say how soon, though. Hope springs eternal.
--George Scialabba
Leave a comment